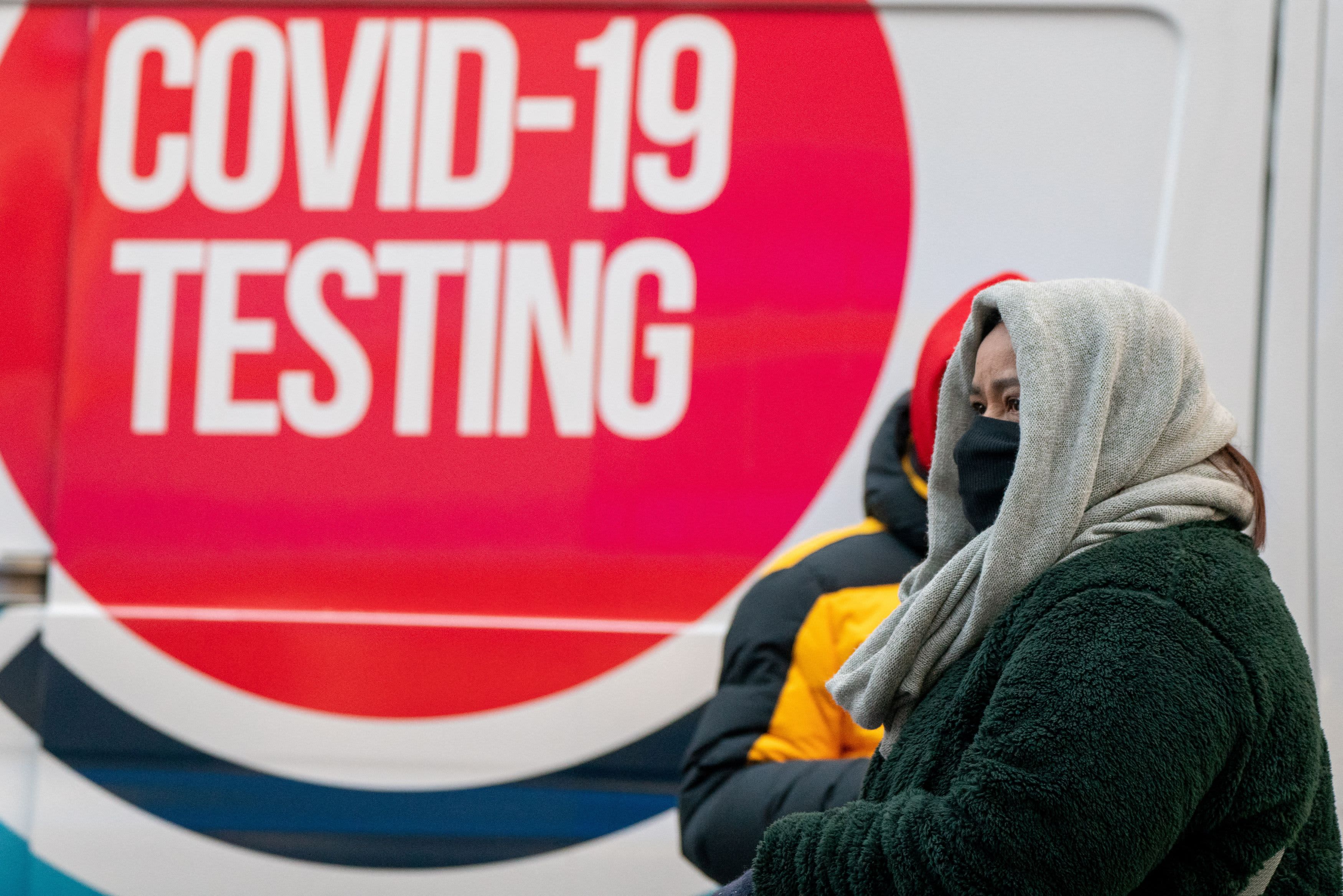
In the midst of Covid’s omicron surge, with tests in short supply, you may be scrambling to figure out the best course of action if you’ve developed symptoms or been exposed to someone with the virus.
Maybe you wonder if it’s worth waiting in line for hours for a polymerase chain reaction (PCR) test, or if you can rely on the results of an at-home rapid test — if you can even get one. Or perhaps you’ve already tested positive, and you need to know how long to wait before you aren’t contagious anymore.
There’s plenty of advice floating around for those types of dilemmas, especially on social media — and not all of it is worth taking. Here are three recommendations from some of the country’s leading microbiologists and infectious disease experts:
1. If you can’t get a PCR, take two rapid tests two days apart.
While the PCR is the gold standard for testing, if you can’t get one, two rapid antigen tests spaced 48 hours apart are an acceptable alternative, says Matthew Binnicker, Ph.D., Medical Director of the Clinical Virology Laboratory at the Mayo Clinic in Rochester, Minnesota.
If you have Covid symptoms like fever, cough, sore throat, runny nose or congestion, but test negative, he recommends that you take a second at-home test in 24 to 48 hours.
“If both tests are negative and symptoms persist or get worse, seek out PCR testing for both Covid-19 and influenza,” he says. If you don’t have symptoms, but want to test after you’ve been exposed, do it on your third and fifth days post-exposure, Binnicker adds.
That reflects the Centers for Disease Control and Prevention’s current guidance, which notes that “repeating the test within a few days, with at least 24 hours between tests, will increase the confidence that you are not infected.”
Multiple tests can’t hurt, even if you feel fine: Repeated rapid testing over multiple days enhances the chances of detecting infection, says Christopher Brooke, PhD, an associate professor of microbiology at the University of Illinois in Urbana, Illinois.
A study Brooke co-authored, published last June in the Journal of Infectious Diseases, found that both PCR and antigen tests can pick up 98% of all Covid cases if they’re done at least every three days.
2. To see if you are infected, take a PCR. Wondering if you’re still contagious? Take a rapid test.
PCR tests are more accurate for detecting Covid than rapid tests. They’re much more sensitive, too — making them the best tests to use to determine infection, says Dr. Scott Roberts, a Yale Medicine infectious diseases doctor and assistant professor at the Yale School of Medicine in New Haven, Connecticut.
But they’re less helpful in determining whether you’re still contagious. “A PCR test will still be positive if dead virus is in your nose, which can last for many weeks after an infection,” Roberts explains. Since rapid tests look for a protein that’s made by an actively replicating virus, it’s a better marker for contagiousness.
If you do test negative, you should still exercise caution, warns Binnicker. A small study released earlier this month followed 30 people who used both rapid and PCR tests at the same time, and found four cases where people still passed the virus to others after testing negative on rapid tests.
That same concept is why the CDC still recommends that you mask up around others for ten days after you initially test positive for Covid, even if you have no symptoms.
3. Swab your nose, not your throat — at least for now.
Advice to swab your throat is making the rounds on social media, but experts are hesitant to recommend this — for now.
One small pre-print study compared the accuracy of saliva and nasal sampling on 382 people with symptoms of COVID-19 who also had PCR tests done. It found that saliva tests picked up 100% of omicron cases, while the nasal swabs only detected 86%.
But there are no known studies that have directly tested nose versus throat for rapid antigen tests. In addition, the at-home rapid tests only received emergency use authorization (EUA) from the FDA as nasal swabs, points out Binnicker.
“A throat swab may yield a false-positive result, since these rapid antigen tests are influenced by the pH (acidity level) in the sample, and your throat pH can be influenced by food and beverages,” he explains.
If you decide to do both, Brooke recommends swabbing your throat first, and then your nose — since the virus sometimes replicates in the throat first before moving into the nasal passages. “The swabbing order is [also] because it seems grosser to swab your nose before your throat,” he adds.
Just keep in mind that this is definitely an “off-label” use that’s not consistent with current FDA guidance, Brooke says.
Sign up now: Get smarter about your money and career with our weekly newsletter
Don’t miss:




